On a cold winter night - we are now in the year 1891 - Bessie Daschle, a calm-tempered lady who is always keen to be elegant, lies on the bed to breathe her last after an intermittent conversation with her physician, Dr. William Bradley Cole (1) , a famous orthopedic surgeon He had tried so hard over the past several months to find a cure for his horrific problem, but he couldn't. Daschle passed away in peace after a bitter struggle with one of the most grueling illnesses, but that particular night Cole is out of the house deciding to leave orthopedics aside and continue the entire journey to understand this deadly beast, Cancer.
As a first step, Mr. Cooley went to the registers of cancer patients in major hospitals to search for any case that had escaped him, and his first observations were a patient from Manhattan who was cured of cancer after contracting a bacterial infection after surgery, here. Our truth-seeking friend traveled to meet the man and make sure he was alive and living the good life, and he did. It was at that point that Cole came up with a strange idea saying that a bacterial infection might stimulate our immune system, so that the latter would attack the cancer and kill it. Others, more numerous, did away with that treatment plan.
But despite that failure, what Cooley presented to the world is a starting point for what happened yesterday, which is the announcement of the occurrence (2) of Dr. James P. Allison of the Anderson Cancer Center at the University of Texas, and Dr. Tasuku Honjo of Kyoto University The Japanese, equating, were awarded the Nobel Prize for Medicine and Physiology in 2018 for their achievements in cancer immunotherapy, as each of them, separately and differently, managed to find a way to raise the ability of our immune system to attack cancer cells, which brought about a revolution in the world of cancer and its treatment, The award culminates in a career of nearly 150 years, from Bradley Cooley to the winning duo.
How our bodies entered the war?
To achieve a better understanding of that idea that at first glance seems unacceptable, and it was indeed so over a wide period of time, let's start with how our body can fight diseases, the moment you read this, there are millions of living things, including bacteria, viruses and fungi, You try to inhabit your body and feed on what has good things, for this reason our bodies have developed a whole army of special cells of various shapes and functions in order to repel this attack, but this fierce war does not begin until after the first important intelligence step, which is to identify the foreign body.
In fact, our bodies have a very ingenious ability to distinguish between what is subordinate to us (I am Self) and what is not belonging to us (I am not Non-Self) from cells, for example a virus or those bacteria that cause a skin disease that are not our own, so let it start The immune system attacks. This intelligence mission is performed by a type of immune white blood cell called "T-cells" (3) , and it does this very brilliantly, so let's imagine, for example, that a virus immediately entered one of your cells, and then began to occupy it through puffs Its nuclear material is in it, which will in turn change the internal environment of the cell. When this happens, some types of receptors on the surface of that cell will change the information it possesses from the inside.
At that point, the T cells appear, which are constantly circulating in the blood and using a technique that we can liken - in a very simple way, the idea may not fulfill its meaning - to the barcode reader of goods in the mall, which passes to read those receptors on the surface of the cells. Every healthy cell gives a specific code that prompts the T-intelligence to give a green light and pass it safely, it is affiliated with us, but when those infected cells pass on the T barcode device, a red light alarm sounds saying: "This cell is not affiliated with us, it contains a foreign body." The immune warfare begins, which includes a counter attack on that infected cell that causes it to die, and then the T cells copy the archives of that war in order to prepare for any upcoming attack of the same type.
For this reason, this chemical relationship, the cellular receptor and the reading barcode, was of great interest in the research community, which in turn caused several previous Nobel Prizes, but the main idea says that these T cells have two regulatory systems, that is, two proteins on their surface, the first activates the T cell to intervene with an attack It is overwhelming, but the other represents the role of the car's brakes, as it prevents it from attacking the cells. This mechanism is what regulates the work of T cells, and between activating and inhibiting the body, standing at the line between self-harm and foreign cell harm.
Our bodies as a weapon against cancer
Of course, the matter is not so simple, but the general idea is the same, at that stage you may begin to ask about cancer, and here let's go back to the similes again. Cancer cells are undoubtedly a war against the body, trying to spread, multiply, branch and control their surroundings, the reason for that will be We talk about it shortly, but what we need to draw attention to here is that many of these cancer soldiers are able, in some way, to wear smart masks that prevent the T cells from recognizing them, as the T barcode passes over the cancer cell, giving it a green signal, to pass safely.
It is precisely at that point that the first (4) winner of the Nobel Prize intervenes . In the nineties of the last century, he was able to discover that it is possible for us - in the laboratory - to develop an antibody to one of the proteins on the surface of the T cell, those that work with the task of "braking", It is called CTLA-4, when we introduce this antibody into the body it does not prevent T cells from carrying out an attack on cancer cells, in other words, it prompts T cells to give a red alert even with cancer cells. The first experiments in animals, and then in humans, succeeded, until 2010, when an important clinical study showed startling effects in patients with advanced skin cancer, and in a group of them, signs of remaining cancer disappeared. Results like this have never been seen before.
On the other side of the world, Hongji was doing the same thing (5) , but with another protein that resides on the surface of the T cell and called PD-1, and he was able with his team to carry out a set of very successful initial experiments, especially since the immune symptoms were less effective than his American companion. In 2012, an important major study showed a clear efficacy in treating patients with different types of cancer. The results were striking, due to the length of time before the cancer recurred again or not at all, and the results were remarkable in the case of patients with metastatic cancer (6) the process of transfer of cancer cells from one organ to another), a condition that was considered Previously not amenable to basic treatment.
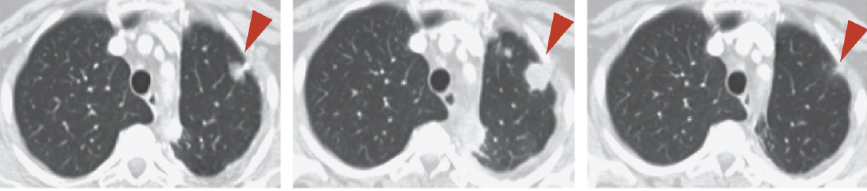 Left to right, within only four months of treatment with pd-1 antagonists, the cancer had ended in lung cancer cases. (communication Web-sites)
Left to right, within only four months of treatment with pd-1 antagonists, the cancer had ended in lung cancer cases. (communication Web-sites)During the past eight years, many new tools have appeared that specialize in treating some types of cancer immunologically, but what is striking has always been the success rates of the combination of the two treatments, as we know that each of them plays a completely different mechanism from the others, therefore merging them together stimulates the attack on cancer cells To better understand this, we can imagine that the CLTA-4, for example, is the "foot brake" and has been stopped, while the PD-1 is the "handbrake" and has also been stopped, pushing the attack on the cancer to its maximum. If the treatment is successful ( 7) Dependent on the work of Allison by 37%, and the other developed by Tasuco by 56%, the use of a drug that brings them together gave a success rate of 68%, and these are great rates with cases that were once without treatment.
Is it a war against the body as well?
In fact, Allison's first intentions were out of tune, because attempts to treat cancer immunologically are not new, for more than 70 years researchers have tried to use the body's own immunity to attack cancer, but most experiments in this area did not succeed, and at some point the conversation was Cancer immunotherapy is the closest thing to a false science, which is why research activities related to this protein, CTLA-4, have been directed towards the creation of drugs related to immune diseases.
In one of his lectures at Barclay University (7) , Allison says, "It was a really strange idea, but it seemed to be worth it." Cancer cells only, in fact perhaps this particular question is what is on your mind during our previous conversation, you might say to yourself: “If we were to disable the T-cell brakes, they would be launched throughout the body to kill cancer cells and normal cells as well, since we destroyed the regulation process that occurs to us About it a little while ago.
But this is not true in the understandable sense, and this is because there is an increasing amount of research data (8) indicating that the immune system, after we turn off its brakes, can devote a major part of its attention to working on the cells resulting from the genetic instability, in the clearest sense: because Cancer - in its roots - is the result of an abnormal mutations process, and as it develops, it continues to generate genetic mutations. The body may cause some side effects related to lung and colon infections, adrenal insufficiency, and pituitary problems.
But with the greater tendency to attack cancer cells, the results were very promising, especially since this type of treatment possesses a second very important feature, which is memory. We learned a little while ago that the cells of the immune system remember the cells that attack them and collect their information and save them an anti-team ready to receive them in Any time, which means a better chance of treating cancer when the patient recedes again, this was one of the most important results of the new treatment in many cases, and the third advantage of immunotherapy is the greater ability to adapt to the future complications of the condition.
Why do not we cure cancer forever and go?
However, at that stage, you must now wonder about all this complexity, and you say, for example, that this previous percentage in the success of the treatment provided by Allison (37%) is a small percentage of this huge celebration, why - this is how many ask - we do not cure cancer? Why is he so stubborn despite all this research over decades? Couldn't we just find one remedy that would do that? In fact, your questions may be logical when we view cancer as one disease, and of course most people think that it has one name, "cancer", just as pneumonia, tuberculosis or malaria have one name. Is not cancer then one disease?
Is not, in fact, the problem begins basically that we talk about "cure" and one for cancer, because cancer does not work one way, of course, the root of the president of the cancer is the disruption of cellular property called "apoptosis cell (9) Apoptosis" From work - for a genetic reason, as we imagine - cells begin to grow in a steady manner, but cancer may develop in different forms and in different tissues, which makes each of its types a specific disease. Therefore, there is a need to search for a cure for each of these diseases, "cancer" then It is the definition of a whole group of diseases that branch, complex and evolve with intensity.
In addition, those mutations that cause cancer in the first place do not occur in the same pattern every time, and as a cancerous tumor develops more and more, new mutations occur that differ from one cancer to another, and from one case to another, which in turn increases the number of possibilities that these mutations gather together, which complicates the situation. The one severely becomes untreatable with time and development at times, for this reason you may find that one treatment may not cause a cure for all cases, the tumor for each of them differs in some way from the other, because each case has its own genetic pathway different from the other.
Knowledge is from the bulk of knowledge
“We got here, not by working on cancer itself in any way, but just by tracing basic research to understand how the human immune system works,” says Alison. “The real surprise is that we were not working,” says Alison.
Mainly on the search for a cure for cancer, but here we are able to develop what is now one of the major pillars of cancer treatment, besides surgical, radio, and medicinal treatment, immunotherapy appeared to come closer to the origin of cancer itself, its genetic makeup we mean.
This idea deserves a little ponder, and it is perhaps the most important thing that we can come out with from Nobel Medicine 2018, as there are two (10) types of scientific research: Basic research does not aim to discover specific drugs, but aims mainly to expand our knowledge on the topic What the research team is studying, for example, the goal of both Alison and Hongji was not to extract a cancer drug, nor to study cancer in the first place, but rather to broaden our understanding of the basic principles of the immune system by asking the basic formulas "why" and "how"?
Basic research, then, is launched only driven by human curiosity towards recognizing things. On the other hand, Applied Research is only launched driven by practical purposes, to produce a specific product, mechanism of action, or new technology to solve a specific problem, such as trying to find a new drug for skin cancer specifically. We know through several studies (11) that 80% of the best drugs that we obtained were carried out by the method of basic research, and although it seems at first glance something to be a fantasy utopian tendency, to search only for knowledge for the sake of knowledge, but the results of this are clear and certain despite the complexities of the situation. Global political and economic, those are the best ways to understand, just follow your curiosity.
Noble Medicine 2018 was not only about the discovery of one person, or research team, of a new door through which we can enter to treat cancer, but it was the result of long-term scientific research that stood on the shoulders of giants (12) beginning with Paul Ehrlich (Nobel 1908), then Frank Bonnet (Noble 1960), Peter Doherty with Rolf Zinkeringal (Noble 1966), George Snell (Noble 1980), George Kohler with Cesar Milsten (Nobel 1984), then Suzumu Tonegawa Nobel (Nobel 1987), and many times that number could not get a Nobel, Little by little, they all contributed to our understanding of our immune system. Such is the science, it may go slowly in many cases, but its results are great.
In the end, the 2018 Nobel Medicine and Physiology 2018 is an important message from the Nobel Authority, especially since this is the first Nobel Prize for a "cure" that was put forward to fight cancer, a message telling patients that there is hope. Patients also, for with the length of time that scientific research took in the fight against cancer, some came out to say that it might remain so, that despair of science led to another wave in which patients left treatment and resorted to folk medicine and pseudoscience, but Nobel 2018 came to say to patients Cancer that there are successful attempts, and unprecedented developments, she came to say to them: "No, wait, do not despair, treatment is coming."